
Pain after surgery
You will have pain after surgery. Together, you and your health care team will create a pain plan that is right for you.
- You and your health care team will also establish a “pain goal” – the amount of acceptable pain you can handle. Your health care team will help you balance your pain so you are able to do your physical therapy and activities of daily living.
Pain scale
Use a number scale (0 to 10) to rate your pain will help the health care team members know how severe your pain is and help them make decisions about how to treat it. 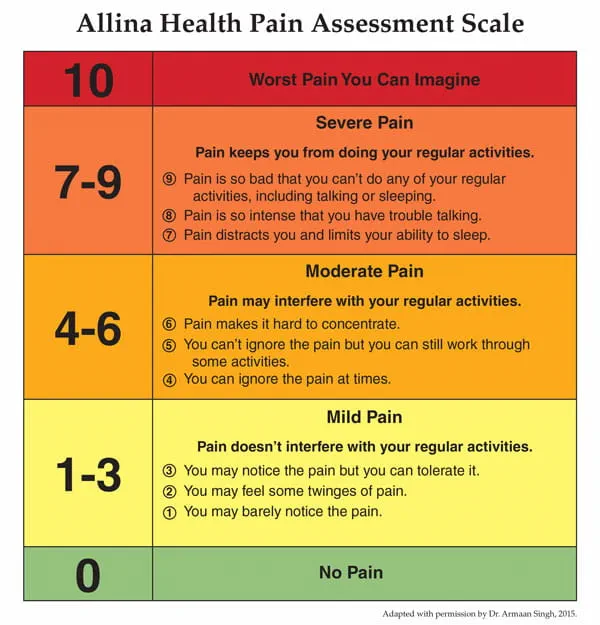
Your role in creating a pain plan
After surgery, it is common to have some pain. A member of your health care team will monitor your pain level often and help you review treatment options.
All of the following information will help your health care provider prescribe the right medicine and therapy for your pain, and prevent serious side effects (complications). Tell a member of your health care team:
- if you have allergies or reactions to pain medicine(s)
- what methods of pain control have worked or have not worked well in the past
- where you feel pain and how much pain you have (use words to describe how the pain feels)
- what makes your pain better or worse
- if your pain starts to get worse or you have new pain
- what vitamins, herbal and natural products you are taking
- if you drink more than two alcoholic drinks each day
Treatments for pain
If you have short-term or sudden pain from surgery, injury or illness, opioid pain medicine may help you to have less pain. Opioid pain medicine is one strategy out of many that you may
use to have less pain and a speedier recovery.
The goal of opioid pain medicine is to reduce pain when it is most intense during your recovery. It is important to switch to non-opioid pain medicines as soon as you are able.
How to relieve pain or discomfort without medicine
Medicines are a great way to relieve pain. However, sometimes they don't last long enough or cause too many side effects.
Your nurse can give you many ways to relieve pain or discomfort that don't involve medicine. Please ask your nurse for more information about any of the following treatments.
Aromatherapy
Aromatherapy uses essential oils to encourage your body's natural ability to relax and heal. Studies have shown that using aromatherapy helps reduce pain, anxiety, upset stomach (nausea) and being unable to sleep (insomnia).
Activity
Spending too much time lying down or sitting in one position can cause pain, muscle cramps or fatigue. Going for a walk can help reduce discomfort and upset stomach. By being active, you shorten your recovery time and you lower your risk for pneumonia, blood clots, and constipation.
Back rub or massage
Massage helps to reduce pain, anxiety, muscle tension and stress.
Effleurage (gentle massage)
Effleurage is a type of gentle massage that involves little to no pressure. It uses gentle strokes on your skin to relax your muscles and helps gets your blood flowing. It is good if you don't like or don't want a regular massage.
Shower
Standing under a hot shower can reduce pain, ease sore muscles and help you relax.
Breathing and relaxation
Your nurse can show you some easy breathing exercises that can reduce pain. This helps lower your heart rate and blood pressure and increase blood flow to your muscles. Relaxation techniques are shown to increase mood and reduce feelings of stress.
Changes to your environment
Simple things like dimming the lights, lowering the curtains, turning off the TV, closing the door or adjusting the temperature in your room can help you rest and relax. These changes can also help if you have headaches or migraines.
Ice pack or frozen gel pack
Cold therapy reduces discomfort and swelling (inflammation) by numbing nerve endings. It can help ease pain after surgery. It can also be used for back pain, arthritis and headaches.
How to safely use cold therapy
- Use an ice pack or a frozen gel pack for 15 to 20 minutes at a time or as directed by your surgeon.
— If you are using an ice pack, put a clean, dry towel between your skin and the ice pack. Do not place the ice pack directly on your skin.
— If you are using a frozen gel pack, put it inside the sleeve pocket given to you before you put it on your skin. Do not place the frozen gel pack directly on your skin. - Wait 90 minutes to 2 hours before you use the ice pack or frozen gel pack again.
- Check your skin color, temperature and sensation before and after using ice packs and frozen gel packs. Do not use cold therapy on red areas or if you have any burning or numbness near the application site.
Call your surgeon if you have any questions or concerns about your skin or how to safely use cold therapy.
Important
Never put an ice pack or a frozen gel pack directly onto your skin. Always follow your surgeon’s instructions to help prevent skin damage.
Change positions in bed
You may not be able to get out of bed. Changing the position of your body in the bed often - every 2 hours - can reduce pain and discomfort. Making sure your hips, back and head are in proper alignment can be a great way to prevent muscle strains, joint or back pain.
A member of your health care team will help you change positions.
Rest
Activity and moving is important for your recovery. However, you may do more activity than your body can tolerate. Allowing your body to rest is also important when recovering from surgery.
Pace your activities and movements with rest. As you recover, slowly do more activities.
Pain management after surgery
These four videos review pain expectations, rating your pain, pain treatment options and home pain management.