
Atrial fibrillation
 Atrial fibrillation is one type of an abnormal heartbeat, causing your heart to beat in an irregular rhythm.
Atrial fibrillation is one type of an abnormal heartbeat, causing your heart to beat in an irregular rhythm.
Atrial fibrillation can occur in people who have a history of heart disease, valve disease, high blood pressure, an overactive thyroid or sleep apnea. Sometimes atrial fibrillation occurs in healthy people. It may interfere with your ability to exercise.
Electrical impulses
The heart is divided into four chambers:
- two upper chambers (atria)
- two lower chambers (ventricles).
The electrical impulse that causes a heart to beat begins in the sinoatrial (SA) node and goes down to the atrioventricular (AV) node. From there, the impulse spreads through the ventricle. This causes a heart at rest to beat between 60 to 100 times per minute.
How atrial fibrillation happens
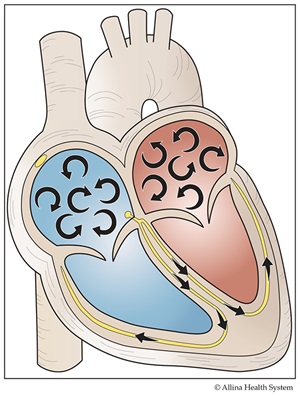
Your heart has four chambers. Two upper chambers (atria) pump blood to the two lower chambers (ventricles). In order for the heart to pump, it requires an electrical impulse to start a heartbeat.
In atrial fibrillation, the atria quiver or fibrillate. The ventricles receive erratic impulses from the atria and so contract in an irregular and uneven pattern.
Symptoms of atrial fibrillation
Symptoms of atrial fibrillation can be steady or they can come and go. They include feeling:
- an irregular heartbeat
- a sense of anxiety
- a tightness in the chest that won’t go away
- tired, rundown, or weak
- short of breath when exercising or working
- palpitations or racing of the heart
- feeling faint
How atrial fibrillation is found
Your doctor will listen to your heart and may give you an exam. Other tests you may have include any of the following.
- an electrocardiogram (ECG): This painless test can be done in your doctor’s office. The ECG shows the electrical flow in your heart. This is recorded onto paper. If you have atrial fibrillation at the time of the ECG, your doctor will be able to tell by looking at the rhythm. You may have atrial fibrillation that comes and goes. You may need to wear a Holter or event monitor for several days or weeks to identify the rhythm.
- a Holter monitor: A Holter monitor helps determine how your heart responds to normal activity. A Holter monitor is a small, portable ECG monitor that records your heart rhythm nonstop. You wear the monitor for 24 to 48 hours. While wearing the monitor, you will keep a diary of your activities and symptoms. Your doctor can compare this to your heart rhythm recordings.
- an event monitor: An event monitor records your heart rhythm for up to 30 days. It helps your doctor diagnose arrhythmias that aren’t common. Your doctor will tell you how long you need to wear one. When you feel symptoms, you push a button. This triggers the monitor to record your heart rhythm for several seconds during your symptoms and after the event. The monitor prompts you to record your symptoms so your doctor can compare your heart rhythm and activity records when you are done wearing the monitor. There are different types of monitors. They will not interfere with your everyday life.
Risks
For most people, atrial fibrillation is not a life-threatening issue. But, it can place you at risk for blood clots and heart failure.
- blood clots: In atrial fibrillation, the upper chambers don’t fully contract (squeeze together). This may cause blood to pool in the atria and blood clots may form.
- If a blood clot travels out of the atrium, it can cause problems with blood flow in other areas of your body.
- If the clot travels to your brain, it can stop the flow of oxygen-rich blood to part of your brain, causing a stroke.
- If the clot travels down a heart artery, it can limit blood flow to a portion of your heart muscle, causing a heart attack.
- Clots can also cause damage to other areas of your body.
Your doctor will talk with you about your risk for blood clots. Things like heart failure, high blood pressure, age, diabetes, and a previous stroke can place you at higher risk. Your doctor may want you to take aspirin or a blood-thinner medicine to help lower your risk.
- heart failure: In atrial fibrillation, your heart rate can be faster than normal. If your heart beats too fast, for too much of the time, your heart muscle can become weak. When your heart loses its ability to pump blood through the body well, heart failure can develop. Symptoms include shortness of breath, weight gain, and swelling in your feet, ankles, legs, or abdomen. Your doctor may want you to take medicine to control your heart rate to reduce your risk of developing heart failure.
Treatment
- medicine:
- anticoagulant medicines: Medicines such as warfarin (Jantoven®), dabigatran etexilate (Pradaxa®) or rivaroxaban (Xarelto®) may reduce the risk of stroke by slowing down the clotting of your blood. Strokes are usually caused by clots that break off and flow to your brain. Aspirin may also be used as part of your treatment.
- rate-controlling medicines: These are used to keep your heart rate in a normal range. You may tolerate atrial fibrillation better when your heart rate is lowered.
- antiarrhythmic medicines (rhythm-controlling medicines): These are used to return your heart to its normal rhythm.
- electrical cardioversion: This uses an electrical shock to return your heart back to a normal rhythm. This can be done with or without antiarrhythmic medicine. You will likely need to take a blood thinner before and after cardioversion.
- electrophysiology study/ablation: This is a study of the electrical system of your heart. Wires are put in your heart through veins. This study may lead to an ablation treatment which may get rid of the arrhythmia. Sometimes this results in the need for a permanent pacemaker.