
Understanding Stroke
By learning about strokes, you and members of your care circle (your family, friends and others close to you) can work toward a better recovery. This information may also help prevent a future stroke.
This written content and videos will provide you with the information you need to know about strokes. Talk with your health care provider about your current health.
Allina Health patient education manual

If you have had a stroke or are caring for someone who had a stroke, we can help.
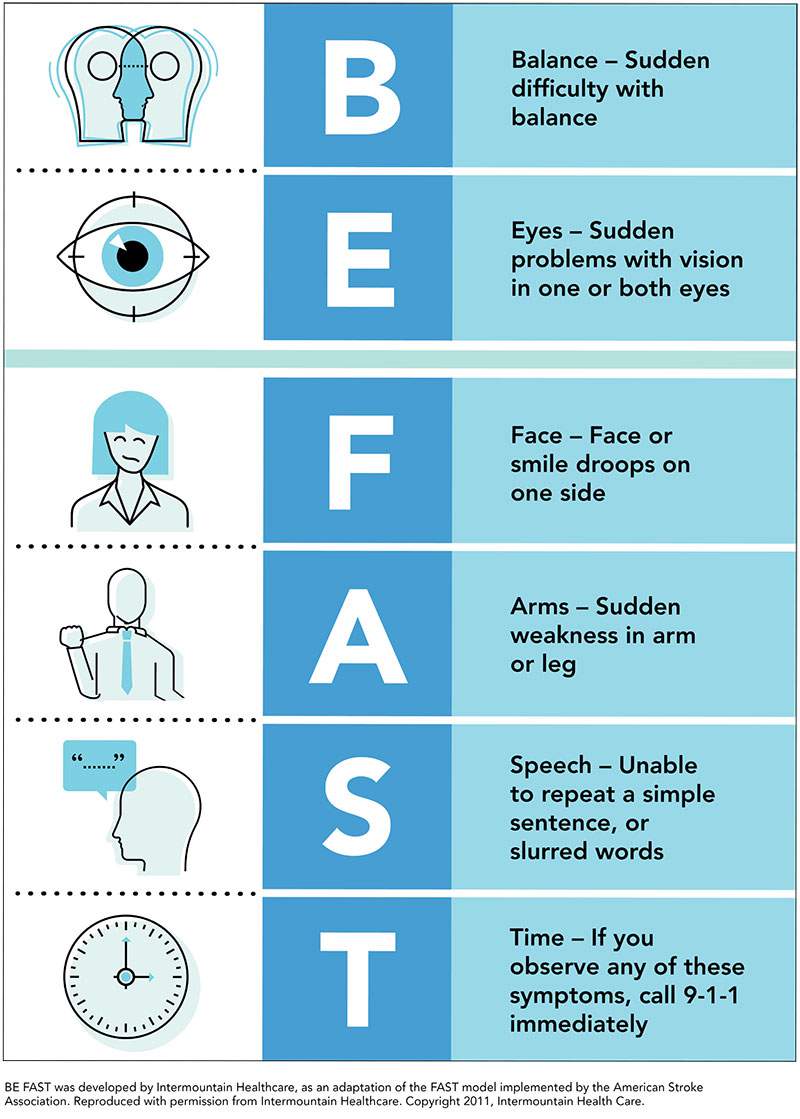
A stroke results when blood and oxygen flow to the brain is stopped or interrupted. This happens because of a ruptured or blocked blood vessel. If you have any stroke warning signs, call 911 right away.
Certain risks increase your chance of having a stroke. There are two types of risks: those you can control and those you cannot. Your health care provider can help you learn what your risks are and how you can control them.
Chapter 2: Your Risks, Prevention and Stroke Signs and Symptoms
Treatment begins in the Emergency Department. The Emergency Department may use a “stroke code.” This code calls a specialized stroke team to your bedside. This process helps you quickly get care.
Taking your medicine as directed is important. Your health care provider will decide which medicines you should take and will give you more information about your medicine.
Rehabilitation usually starts in the hospital. You may continue with it after your hospital stay. Together, you and members of your health care team and care circle will make rehabilitation choices before you leave the hospital.
Your stroke may affect how you think, move, feel, or a combination of these ways. Changes after your brain injury may be short-term or long-lasting. Changes may range from mild to severe.
Your loved one may or may not want to have visitors during his or her hospital stay. Respect your loved one’s wishes about when he or she would like to see members of his or her care circle.
List of Allina Health resources, community resources and support group information.
Patient education videos
Explore the video library for trusted, easy-to-understand health and wellness education. View video library stroke topics.
If you would like a printed, spiral-bound copy, please fill out online form.
View list of manuals and prices. All sales are final.
Related Allina Health resources