
Pain medicine
Anesthesia pain relief during labor
You will have different pain relief options available to you during labor. This video explains those options and how they may change, depending on your medical condition.
During your labor, you'll have different pain relief options available to you. These options may change depending upon your medical condition.
During a normal vaginal delivery, one simple option is to administer pain medication through your IV. The IV pain medication may be enough to lessen the pain as you go through the first and second stages of labor.
There are times, however, when you will feel that more pain relief is needed than what you're getting from the IV pain medication. In these cases, a procedural called an epidural can be done. An epidural is a procedure where a small tube will be placed through the skin of your back using a needle. The needle's then removed, and special pain medicine's given through that tube to provide you with a higher level of pain relief. This medicine's typically delivered right up until the baby is delivered.
Even if you want to give birth vaginally, there are times when it may be necessary for your obstetrician to recommend delivery by Cesarean section. If you already have an epidural in place, this will most likely be used to give you additional medicine so you don't feel any pain during the surgery.
If you're scheduled for a Cesarean birth in advance, or a Cesarean birth is recommended while you're in labor but you don't have an epidural in, you'll most likely receive spinal anesthesia. Spinal anesthesia's an injection of medicine through the skin of your lower back. This medicine will make the lower part of your body numb, temporarily, so you don't feel any pain during the surgery.
There are rare times when it might be necessary for you to receive general anesthesia for your Cesarean birth. General anesthesia's where you're given medicines through your IV, and these medicines will make you go off to sleep for the surgery. Anesthesia medicines will be continued that will keep you asleep until the surgery's completely done.
Regardless of the kind of anesthesia that you have for your Cesarean birth, you will receive pain medication to help you to feel as comfortable as possible after the surgery.
We at Allina Health are fully committed to seeing you through the birth process as comfortably and safely as possible.
Pain medicine
Medicines can be valuable during labor. They can reduce or relieve pain. Some help you work with your contractions. Others allow you to rest. The choice of what you use is a decision you and your health care provider make together. Weigh the advice of your nurse or health care provider with your own preferences.
Your baby may be affected by medicine you take. How much your baby is affected depends on the kind of medicine, the timing of the medicine and the dose.
If enough time passes between when you receive the medicine and when your baby is born, your body will process the medicine. That results in the medicine having less effect on your baby at the time of birth.
Questions to ask
- How is the medicine given?
- How soon can I get it?
- How long will it take for the medicine to take effect?
- Does this medicine relieve pain or reduce it?
- How long does it last?
- Can I get another dose if I need it?
- How will the medicine affect me?
- How will the medicine affect my baby?
Deciding to use medicine
Most health care providers feel that pain medicines won't slow labor. However, you may choose to hold off on taking medicine until you feel you can no longer work with your contractions and you can't rest between them. Take medicine before you exhaust yourself fighting the contractions because this also slows labor as well as wears you out.
When you start having trouble dealing with contractions:
- Change what you are doing during the contractions.
- Change your breathing pattern.
- Change your position.
- Make the room brighter.
- Focus on your partner's face or eyes during the contractions.
- Ask your partner to do more, such as breathe with you or push on your lower back.
- Focus on relaxing between the contractions.
- Use your relaxing breathing between contractions.
- Ask your partner to do things that have helped you relax in the past.
- Use a warm pack or blanket to help your muscles relax.
- Use the warm water of a shower or bath to aid relaxation.
- Ask your nurse for help.
- Ask if your cervix can be checked so that you know how far dilated you are.
- Ask for comfort suggestions.
If you aren't able to get into a new rhythm to cope with the contractions, ask what comfort options are available to help you during delivery.
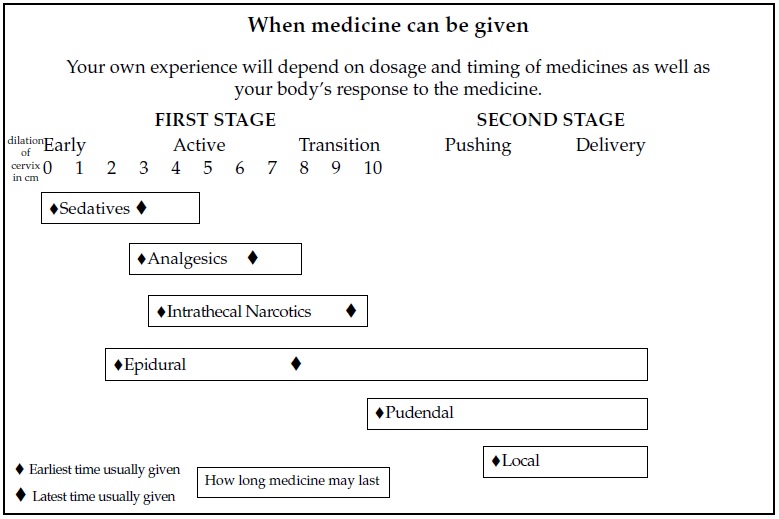
Pain medicines used during labor and birth
Not all the medicines listed in the chart are available at all hospitals. They are also not used by all health care providers. Talk with your health care provider about which medicines might be used during your labor and birth.
When your health care provider suggests a medicine, it is always OK to ask what the benefits and risks might be.
| Medicine | Purpose | Method | Effects |
|---|---|---|---|
| Sedatives | To relieve anxiety, to help you work with contractions, and provide rest when you are exhausted and labor is not well-established. | By injection or pill; takes effect quickly; lasts for several hours; ordered by a doctor or a midwife. | Has little effect on your baby. If you don't want to sleep, you may not like the drowsy feeling. |
| Analgesics | To reduce and relieve pain and help you relax between contractions; you'll still feel contractions, but this "takes the edge off." |
By injection or through intravenous line; takes effect very quickly; lasts up to two hours; ordered by a doctor or a midwife. |
May slow your baby's activity and responses. You may feel dizzy or like you are floating; may slow labor for a short time. Effects on your baby can be reversed with medicine after your baby is born. |
| Epidural | Decreases your sensation of contractions and reduces your pain from just below the breasts to your toes for labor and birth; you'll probably still feel touch, movement, and pressure; you will still be able to move your legs; you can stay alert but can also rest or even sleep. |
An anesthesiologist numbs the injection site, then places a small catheter in your back and medicine flows through it into the epidural space; takes effect within five to 20 minutes; lasts as long as needed; you may feel pressure or a brief feeling like a "shock" down your legs when the catheter is inserted. |
Requires an IV, which you'll have for the rest of labor and birth; your blood pressure may drop; fetal monitoring will be used; you may feel numbness or tingling in your legs; you'll have to stay in bed and may have a bladder catheter; you have a chance of spinal head-ache/nausea; has little effect on your baby's responses after birth. You can't eat or drink once it's in place. |
| Intrathecal narcotics |
Reduces pain, but you will feel touch and pressure; you may rest or get up and walk. |
An anesthesiologist numbs the injection site, then injects the medicine into your spinal fluid; takes effect within five minutes; lasts one to two hours; can be repeated once before second stage. |
May lower your blood pressure and respiration, so there will be regular checks; you may be asked to breathe oxygen by mask or receive medicine to increase your blood pressure; for the first 30 minutes, an electronic fetal monitor will be used—after that, you can walk; you may feel nauseated and itchy; has little effect on your baby's responses after birth. |
| Pudendal | Numbs the vagina and perineum so you don't feel the episiotomy, forceps, or vacuum extractor. |
Injection into the sides of the vagina; takes effect fairly quickly; lasts for a short time after birth; given by a doctor or a midwife. |
You will still feel contractions but may have less of an urge to push; usually has no effect on your baby. |
| Local | Numbs the perineum for episiotomy and episiotomy repair. |
Injected into the perineum; takes effect fairly quickly; lasts for a short time after birth; given by a doctor or a midwife. |
Does not affect your baby. |
The pain medicine for labor and birth chart is also available as a PDF.
Some Allina Health hospitals offer nitrous oxide sedation to help manage labor pain. Nitrous oxide is a medicine given to make you comfortable, relaxed and drowsy for a procedure. Talk with your health care provider if you want more information about nitrous oxide.
Mother baby care
A wide variety of videos on topics ranging from labor and delivery to newborn and postpartum care can be found on our Allina Health mother baby care video page.
Giving birth: Managing pain
- Cesarean birth (five video topics)
- Vaginal birth (five video topics)
Breastfeeding
Breastfeeding your baby is available in English, Arabic, Hmong, Russian, Somali and Spanish.